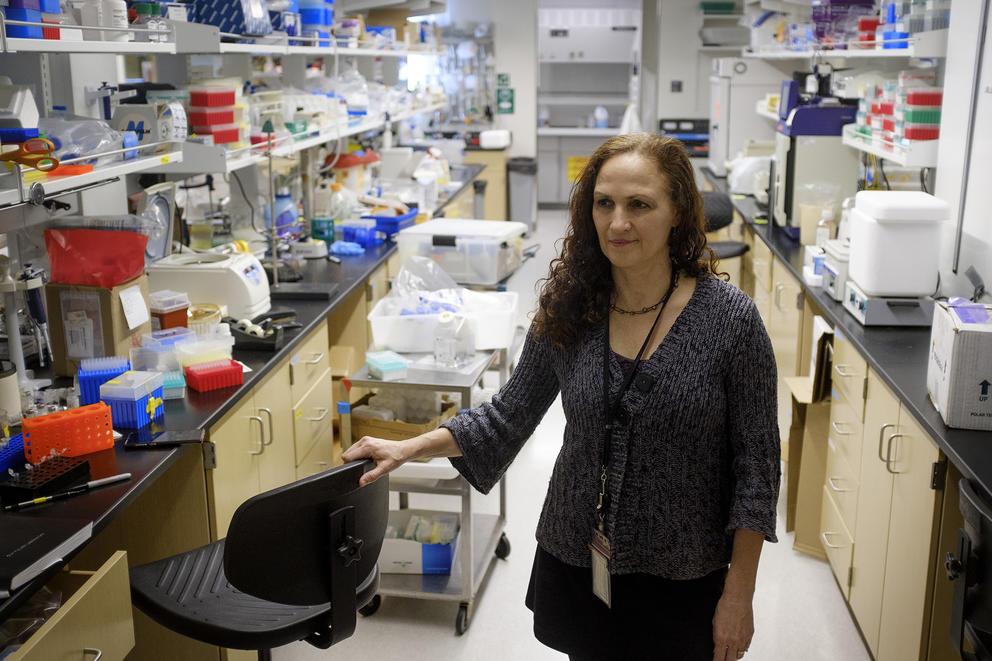
Fuller has been working on vaccines since 1991, specializing in novel DNA and RNA vaccines to spur the antibodies that fight viruses in humans. She and her team believe that this type of vaccine is our best chance at developing a safe vaccine years more quickly than usual, but no DNA or RNA vaccine has ever gotten far enough in human trials to be approved for broad use. As their expertise rockets to the forefront of scientific need, more scientists are testing the DNA/RNA approach. Moderna, the Boston-based company that this week started the first phase one clinical human trial of coronavirus vaccines in Seattle, employed an RNA vaccine.
READ MORE: Coronavirus turns Seattle into America’s laboratory
Here Fuller shares more about this vaccine, how the development process is going and how it feels to be a scientist living at the U.S. epicenter of a historic outbreak.
What does it mean to be a coronavirus vaccinologist right now?
When there is an outbreak like we have now with the coronavirus, my lab gets right on top of that. We’ve been particularly interested in developing technologies that could rapidly respond to an emerging pandemic, especially in the context of flu. I hadn't really studied coronaviruses before, but we always say if you're a vaccinologist you kind of get in bed with whatever virus or parasite happens to be circulating at the time, and so I've worked with malaria and hepatitis B and HIV and influenza.
How do you approach developing a vaccine for a new infectious disease?
First you have to know what the pathogen is and how it works, which is not always obvious when an epidemic is unfolding. With the coronavirus, they were able to identify the sequence of that pathogen very quickly.
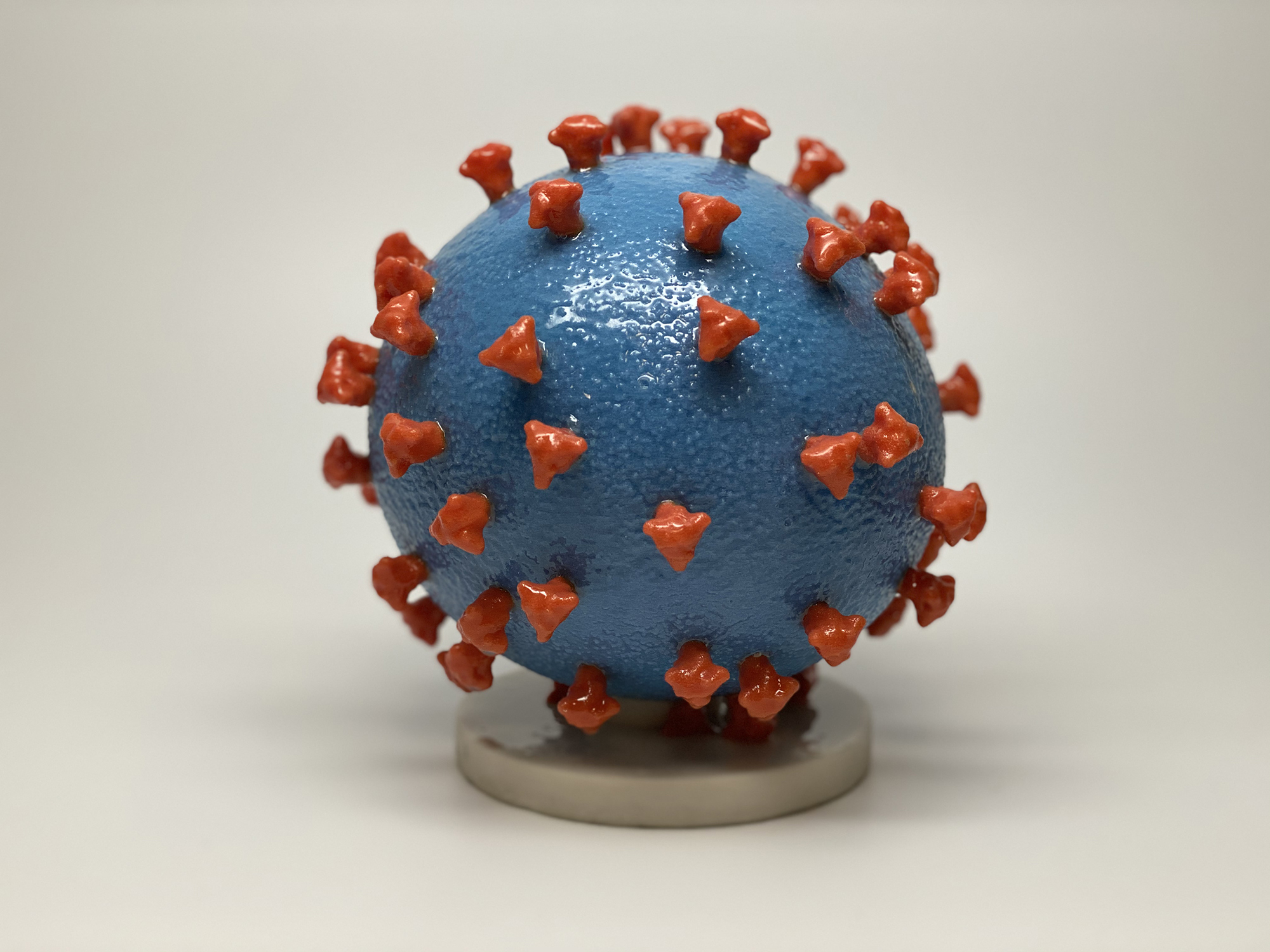
The second part is you need to understand what kind of immune responses are able to protect against that virus. Most often that's going to be an antibody response, and the way antibodies work is that they decorate the outsides of the pathogen, or the virus, and prevent the virus from being able to infect your cells.
And then finally you need technologies capable of inducing that type of immune response at the right time, and so that's really where my lab comes in. You need to have antibodies there right at the time to protect someone, depending on how quickly the virus causes disease.
Prior to the late ’80s and early ’90s, most vaccines fell in three categories: live attenuated like measles, which is a weakened virus that induces an immune response but doesn't cause the disease; or a killed virus like flu, where you just shake and bake it and inject it to create that immune response. There’s also a recombinant protein vaccine like for hepatitis B, where you take a component of the virus — maybe one protein — and you make a recombinant protein and inject it into people and they make an immune response against that protein.
What makes DNA/RNA vaccines — nucleic acid vaccines — so different?
They were [an] entirely new concept. We’d just take the genetic material from the pathogen that encodes, say, a protein, and instead of producing it in a dish and then injecting that into you, we inject the genetic material directly into the cells of a person's skin, and your skin cells start to produce that protein, and it makes the body think it's infected but it's not.
In the case of coronavirus, it's an antibody response against a spike protein, so all you need is this genetic sequence for the spike protein and we can then put that into our RNA or DNA expression cassette, and we've got a vaccine right there! So with respect to what we're actually testing right now, it's really various versions of the spike protein. We need to make sure it's presented to the immune system in the right way to induce the right types of antibodies.
This is exciting for a couple reasons. All those other kinds of vaccines [require more time]. Whether it's a live attenuated one, where you have to figure out mutations that are going to weaken [the virus]; or a killed one, where you’ve got to inactivate it to make sure there's no live virus still in there; or a recombinant protein vaccine, where you’ve got to go through this long protein production process. We skip all that. We just take the genetic material and let you produce the vaccine, in your own body. And so it makes it very, very fast.
For example, our current flu vaccine — from the time that they know what [flu] virus is circulating to the time they actually have a vaccine ready to go — takes at least nine months. With DNA or RNA vaccines, it cuts that short to less than three months.
We’ve also discovered that they induce unique immune responses that other types of vaccines don't always induce, like T-cell responses that help to clear the infection. So if the antibody isn't as effective as you'd like and the virus still sticks around, then you've got these T-cells coming in to eliminate the rest of the infected cells.
If you don’t understand what kind of immune response is going to protect against the virus, that means that DNA or RNA vaccines are going to have a lot more flexibility in terms of the types of pathogens you could go after. They induce both arms of that immune system.
Coronavirus seems to have this bizarre pattern where people have had to quarantine for two weeks to be sure that they've gotten rid of it, so that's a window of time that you could potentially administer it to people recently exposed and be able to induce the immunity sufficient that you clear the infection before they experience really bad signs of disease.
Why don’t we have these nucleic acid vaccines yet for humans?
Back in the early ’90s, when we first started seeing data from nucleic acid vaccines, everybody thought that was just going to revolutionize vaccines. It could replace any other kind of vaccine out there and it would be completely safe because it doesn't have any live component left in it or anything like that.
But the problem was in about the mid-’90s, the first vaccines went into clinical trials, both DNA and RNA vaccines, and they failed miserably. They didn’t create good immune responses. So everything looked great in a mouse and nothing worked in a human. And so everybody got into nucleic acid vaccine research and then most people got out. My lab kept working on it because we figured, well, let's solve this problem.
Flash forward to present day, and we have solved a lot of those problems. There are numbers of them in phase 2 and phase 3 clinical trials, and they do have DNA vaccines licensed for veterinary use. We've demonstrated now that nucleic acid vaccines do work very well in humans [against things like hep B and influenza]; they cause no adverse reactions, they induce strong immune responses and induce protective levels of immunity, and so I think nucleic acid vaccines are back in the game.
How difficult are coronaviruses to develop vaccines for?
I would say they seem a lot easier because it's actually well known that antibodies can protect against a coronavirus. It doesn't have the level of variability that HIV does. So when we talk about a rapid response vaccine, when all those pieces are known, we can just plug in the [antibody-stimulating] antigen that we know would confer immunity in humans into our technology, and we can rapidly test that in mice and then preclinical models like a monkey and then, if that's successful, go right into human trials. It's a good example for us to really put our platforms to the test here.
When did you start working on a coronavirus vaccine?
Within about a week after the sequence was published. We were in a position to start generating and what really got me going was, there is this postdoc [Jesse Erasmus] that had just joined my lab. He comes in and he's like, "So this coronavirus thing, could we make a vaccine for it?" And I was like, yeah, we could probably do that. He was on it right away.
All the pieces are there: We know what immune response is needed, we know what the antigen we need to encode with our vaccines is, and we have the vaccine technologies to do it, so let's run with it and see what we can do!
Where are you in your research?
We've gotten additional data from the mice that passes a benchmark that shows that the antibodies that are being induced are definitely very potent against the virus, so that's promising. But again it's still just mice, so our next step — we're very close — is to start to immunize the monkeys. We've just gotten our protocol through to start monkeys [with an RNA vaccine]. I think we should be able to start the immunizations [this] week on the monkeys.
There’s a lot we still don’t know. We're just getting data for the mice to say, if we induce these antibodies, do they stick around or do they disappear quickly? We don't want them to disappear quickly; otherwise you won't have immunity for very long.
What you want to see is that after we give that one shot, we find really strong antibodies after two weeks. Are they still there after four weeks, and six weeks and 12 weeks, in a year? We don't know yet. But the DNA/RNA vaccines can stimulate that cellular immunity, which might be the backup plan, if the antibody doesn't end up blocking the infection.
How long would a coronavirus vaccine work?
Viruses are tricky. It's constantly a war between the human body, the human immune system and the virus. The virus tries to quickly mutate to evade the human immune response, so it makes an antibody against this spike protein; eventually, the virus is going to want to mutate that [protein] to survive to get away from the antibody. Once it mutates and the antibody doesn't see it anymore, now the virus can keep going on.
Our first coronavirus candidate is based entirely on the original sequence, so if the virus undergoes sufficient genetic mutation in the area that the antibodies are targeting by our vaccine, it's quite possible that then it won't be as effective. It's something we have to keep our eye out for sure.
What has your life been like since the outbreak?
It’s been kind of crazy. We're running around with our pants on fire. It’s kind of like a race, but it's not a race against other scientists: It's a race against the virus.

Does fighting this virus feel different than other pandemics?
I have done vaccine studies to address pandemics in academics before, like Zika and the 2009 H1N1 flu, and this one just feels so much different because it's heightened 10 times more than any other one, and we're living it as we're trying to race against the pandemic and come up with interventions that are going to help. We're thinking about how to package this differently at the same time as we're thinking about how to make the overall vaccine itself work better and more durably! So you can just feel all of the energy in the lab.
It's kind of exciting in a way, it's kind of like when you watch those [pandemic] movies where you see all the lab people in there night and day; it's like that. They got that part right even if they didn't get some of the other parts right.
Everybody's working at a frenzied pace. It's like a whole community is trying to do what they can to help out.
We all feel that we have a particular responsibility because this is where the virus was first detected in the United States, and so there's a lot of motivation there. You want to support other researchers who have other tools, and hope that one or more of these are successful.
How likely is it that we’ll get a vaccine quickly?
I'm actually very optimistic that we're going to have vaccines for coronavirus. Where the challenge is, is how to get them through this whole system quicker. But we can't compromise the safety. That's what holds things up, and figuring out how to scale up and manufacture something.
The typical vaccine development pathway is — and this is terrible — but it usually takes an average of 10 years from the time you first discover a new vaccine in your lab to the time that you actually have it licensed for human use. There's a lot of steps involved. We go through the initial discovery phase [with mice], and then with larger animal models. We go through a long preclinical process and then three phases of human trials.
Phase 1 is just to say, in a small number of people, is it safe? Vaccines have to have maximum benefit with minimum risk. Phase 2 uses a larger number of people, where you again test more safety measures but you also start to test for things like, is it inuring immune responses that we expect? What is the optimal dose that we need to give people? And then if that's successful, then you're going to go into phase 3, which uses a larger population and actually tests it for efficacy. If this coronavirus were still around in a year or two, and we're getting to phase 3 trials, then we'll be able to actually start testing it in thousands of people.
But we're not done yet! Even if you've got a vaccine that looks successful in phase 3 clinical trials, you have to figure out how you're going to manufacture that and scale it out for widespread distribution worldwide, and that's not a trivial process. And then you have this whole regulatory thing with the [Food and Drug Administration].
We need, I think, to find quicker ways to get vaccines into people. We don't necessarily have to immunize the entire population to control an epidemic. We could get past that phase 1 safety trial, and if there's a global pandemic going on and we've shown it's safe and it works in animal models, could we at least vaccinate first responders and people who are closest to those who are infected?
That’s a process called ring vaccination. They’ve been using that since the 1800s. If you build a wall of immunity around an infected population the virus doesn't have anywhere to go past those folks. You could use ring vaccination and then once you really have a licensed vaccine that could be distributed worldwide, then you're going to be relying on things like herd immunity where you get, you know, 60% or 70% of the population vaccinated, and that's going to limit the ability of that virus to ever spread again.